Gastroesophageal reflux disease (GERD) is a condition where stomach acid consistently flows back into the esophagus, the conduit linking your mouth and stomach. This process, known as acid reflux, can cause irritation and damage to the esophageal lining.
While occasional acid reflux is a common experience for many, persistent and frequent reflux can escalate into GERD, leading to more serious health issues if left unaddressed.
Recognizing these indicators is crucial for timely diagnosis and management, especially if you want to avoid emergency medical care.
People with acid reflux might think that other symptoms happening at the same time are just part of reflux. But if you’re having symptoms that are more than just the usual heartburn, it’s not something to ignore. These extra symptoms could be a sign of a more serious problem, so it’s important to take them seriously and possibly check in with a doctor.
These symptoms accompanying acid reflux (or any time) should always mean a trip to the emergency room:
Even if it is not a heart attack, it could be angina or another issue that needs to be addressed quickly.
If you’re dealing with an acid reflux flare-up, it can feel quite uncomfortable. However, there are steps you can take to feel better. Here’s what you can do:
Maintain an Upright Position: Stay seated or standing to use gravity to your advantage, preventing stomach acids from rising.
Identify and Avoid Trigger Foods: Steer clear of known irritants like spicy foods, citrus, and caffeine which can exacerbate reflux.
Opt for Smaller, Frequent Meals: Eating large meals can increase stomach pressure; smaller meals reduce this risk.
Elevate Your Bed: Raising the head of your bed can prevent acid from flowing back while you’re lying down.
Stay Relaxed: Stress can worsen reflux symptoms; find calming activities that work for you.
Avoid Lying Down After Eating: Wait at least two to three hours before lying down to prevent acid from moving upward.
Consult a Healthcare Professional: If attacks are frequent or severe, seeking medical advice can provide you with tailored strategies and possible treatment options.
When in doubt about acid reflux, it is always better to be cautious and get it checked out at The Emergency Center, which has the tools and experts needed to determine the right diagnosis and start treatment.
The Emergency Center has diagnostic capabilities like ECG and advanced CT imaging to diagnose or rule out heart attack. Additionally, with an onsite lab and pharmacy, patients can find answers without the wait and get needed prescriptions before leaving. Whether it ends up being just a bad case of heartburn or something more serious, getting evaluated is the first step in finding both care and something equally as important: peace of mind.
GERD can have various causes and triggers that contribute to the weakening of the lower esophageal sphincter (LES) and the onset of reflux symptoms. Understanding these factors is essential for managing the condition on time.
Here are some of the most common causes and triggers:
If you suspect you have GERD, feel free to complete this quiz so you can be more informed about your symptoms and current condition. Remember that this is only a general quiz, we still recommend visiting a doctor.
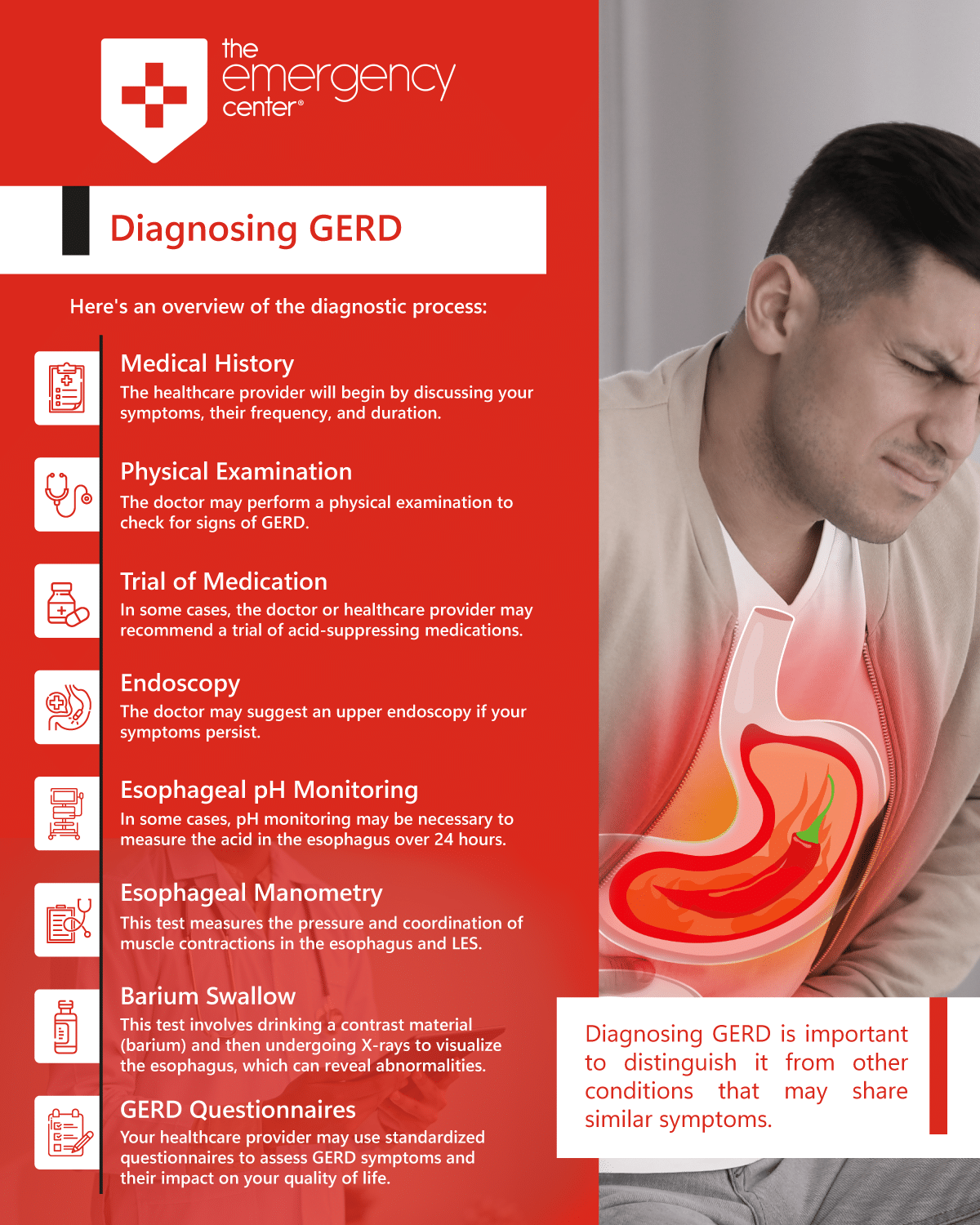
Diagnosing Gastroesophageal Reflux Disease (GERD) involves a combination of medical history assessment, physical examination, and, in some cases, specific tests to confirm the diagnosis and assess the severity of the condition.
Here’s an overview of the diagnostic process:
Medical History: The healthcare provider will begin by discussing your symptoms, frequency, and duration. They will also inquire about your lifestyle, eating habits, and any medications you may be taking.
Physical Examination: The doctor may perform a physical examination to check for signs of GERD, such as listening to your chest and throat for unusual sounds or examining your throat for irritation.
Trial of Medication: In some cases, the doctor or healthcare provider may recommend a trial of acid-suppressing medications, like proton pump inhibitors (PPIs) or H2-receptor antagonists, to see if symptom relief occurs. If symptoms improve with medication, it can provide further evidence of GERD.
Endoscopy: The doctor may suggest an upper endoscopy if your symptoms persist. During this procedure, a flexible tube with a camera (endoscope) is inserted through the mouth and into the esophagus and stomach. This allows the doctor to visually inspect the esophagus for signs of inflammation or damage.
Esophageal pH Monitoring: In some cases, pH monitoring may be necessary to measure the acid in the esophagus over 24 hours. This test can help confirm the diagnosis and assess the frequency of acid reflux.
Barium Swallow: This test involves drinking a contrast material (barium) and then undergoing X-rays to visualize the esophagus, which can reveal abnormalities.
GERD Questionnaires: Your healthcare provider may use standardized questionnaires to assess GERD symptoms and their impact on your quality of life.
Managing Gastroesophageal Reflux Disease (GERD) involves lifestyle changes, medications, and, in severe cases, surgery.
Bile reflux, while often associated with acid reflux, is a distinct condition that deserves attention, especially when discussing serious symptoms of acid reflux. Unlike acid reflux, which involves the backflow of stomach acid into the esophagus, bile reflux involves bile—a digestive fluid produced in the liver—flowing into the stomach and esophagus. Here’s what you need to know about bile reflux within the context of acid reflux disorders:
Distinct Symptoms: Bile reflux can cause a persistent cough, hoarseness, and episodes of nausea, distinguishing it from typical acid reflux symptoms. If you’re experiencing these alongside traditional acid reflux signs, it could indicate bile reflux.
Potential for Damage: Just as stomach acid can erode the esophagus in acid reflux, bile can damage the lining of the stomach and esophagus, leading to serious conditions like Barrett’s esophagus or esophageal cancer.
Diagnostic Importance: If your acid reflux treatments aren’t working, or if you’re experiencing unusual symptoms, it might be time to investigate bile reflux. This condition often requires specific diagnostic tests, such as endoscopy or bile monitoring techniques.
Complications arising from untreated or poorly managed Gastroesophageal Reflux Disease (GERD) can severely impact a person’s health, hence the importance of staying alert to the initial symptoms.
Let’s check the outline of potential complications and the long-term outlook associated with GERD:
Untreated GERD can lead to inflammation of the esophagus (esophagitis), which may cause pain, difficulty swallowing, and, in severe cases, bleeding or ulcers in the esophageal lining.
Repeated exposure to stomach acid can result in the narrowing of the esophagus (strictures), making it difficult to swallow.
We’ve already mentioned this condition before, as it’s probably one of the most common regarding GERD. It happens when chronic acid reflux causes changes in the cells lining the esophagus. Barrett’s esophagus is a risk factor for esophageal cancer, although the risk is relatively low.
GERD can trigger or worsen respiratory conditions such as asthma, chronic cough, and pneumonia due to constant inhalation of stomach contents into the lungs.
The long-term outlook of GERD depends on the severity of the condition, the effectiveness of management, and the presence of complications. You can manage their symptoms effectively and prevent complications with proper treatment and lifestyle adjustments.
However, regular monitoring and follow-up with a healthcare provider are essential to ensure the best possible long-term outcome.
In conclusion, understanding the serious symptoms of acid reflux and GERD is crucial for timely intervention and treatment. While heartburn and regurgitation are common signs, the presence of symptoms like chest pain, difficulty swallowing, and nighttime disturbances signals the need for a more in-depth evaluation. Knowing when to seek emergency medical attention is essential, especially when symptoms mimic those of more severe conditions. Proactive management through dietary adjustments, lifestyle changes, and medical treatment can significantly mitigate the risks associated with GERD. Remember, maintaining open communication with your healthcare provider and addressing symptoms early can prevent the progression of GERD and ensure a better quality of life.
The Emergency Center
San Antonio
11320 Alamo Ranch Pkwy
San Antonio, TX 78253
Phone: 210-485-3644
Conroe
4019 I-45 N,
Conroe, Texas 77304
Phone: 936-247-9457
Is your nausea more than just an upset stomach? Learn about the causes of nausea…
Experiencing numbness or tingling? Discover the causes and know when to seek emergency care for…
Experiencing abdominal pain? Learn what it could mean by location and when to visit the…
Is your skin redness a sign of something serious? Learn about different types of skin…
Why are ER wait times so long? An emergency room physician explains key delays and…
Are you aware of the dangers of carbon monoxide? Learn prevention tips, symptoms, and how…